Health care workers are the frontline of the battle against COVID-19, placing upon their shoulders unprecedented levels of stress, anxiety and grief. Throughout this prolonged crisis GNYHA member institutions have worked to address these needs often pivoting or enhancing existing structures and resources. And this work will continue as we move into new phases of this response.
Below we offer key approaches for considering this work including:
- Resources for ongoing support of staff wellbeing while shifting to routine operations and maintaining COVID-19 capacity
- Phase of response based on number of COVID cases within a particular facility or health system
- Priority aims in meeting hospital staff needs with examples from GNYHA members
- Considerations for distinct parts of the workforce
This information is designed to inform ongoing support efforts in the New York region, as well as across the country. We have also provided a curated list of resources for member hospitals.
Resources for Ongoing Support of Staff Wellbeing while Shifting to Routine Operations and Maintaining COVID-19 Capacity
As COVID-19 positivity rates, cases, and hospitalizations continue to decline, hospitals are shifting their focus back to routine operations, while also remaining vigilant. However, staff throughout the organization may be experiencing exhaustion and anxiety due to the acute and chronic stressors brought on by the COVID-19 pandemic. To support member efforts in this area, GNYHA has curated these resources
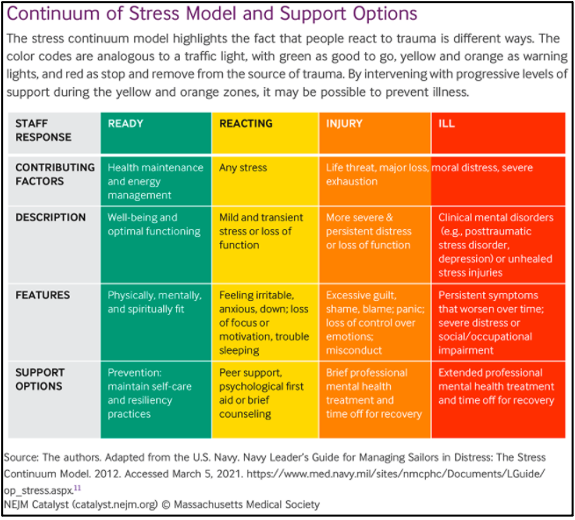
Many healthcare organizations are re-evaluating and working to strengthen their workforce health and wellbeing programs, with a deliberate focus on mental health needs. Like physical health, it is important to meet the needs of staff along a mental health continuum as illustrated in the model below.
Phase of Response
Hospital and health system workforce needs will likely vary based on the phase of the COVID-19 response as described below.
- Early Phase: A single or small number of COVID-19 cases identified. Hospitals anticipate fast shifting caseloads and ICU areas suddenly filling up. There may be anxiety about not knowing what is to come. With limited time to plan, many staff may report not feeling ‘prepared’ for the outbreak. There may be frustrations and confusion as staff quickly adapt to the changes. Disagreement over the sense of urgency may arise.
- Mid-phase: Many new cases daily. There may be strain in technical capacity due to insufficient equipment, staffing shortages, and redeployment anxiety. Health care staff may have increased exposure to experiences that create moral or ethical distress. Staff may experience anxiety about risk to self and others, especially loved ones.
- Acute phase: There will be case overload. Staff may experience increased exposure to the distress of other people. Feelings of powerlessness, distress from inability to provide help at the level and at the time that it is needed, and potential fear of reprisal relating to difficult decisions, may arise. Challenging ethical decisions may arise and support from regulatory organizations, experts, and senior staff may be needed.
- Tail-off phase: Number of cases declining. Some staff may be ‘running on empty,’ and many may experience burnout and retrospective guilt.
- Maintenance phase: Active cases still exist, and capability in case of resurgence must be maintained. Strategies to mitigate staff distress and/or burnout will likely be necessary.
Below are phase-based resources on response that members may find helpful:
| Resource Title | Organizational Author or Journal Title | Description |
|---|---|---|
| Optimizing Staff Preparedness, Wellbeing, And Functioning During The COVID-19 Pandemic Response | Cole King et. Al 2020 | Guidance outlining challenges that health care providers will experience based on severity of the pandemic and intervention and preventive strategies for health care leaders to optimize staff wellbeing. |
| The Psychological Needs of Healthcare Staff as a Result of the Coronavirus Pandemic | British Psychological Society COVID-19 Staff Wellbeing Group | Guidance for health care leaders to address wellbeing of health care staff (clinical and non-clinical) as they respond to COVID-19 from an individual, management, and organizational level. |
| Advice for Sustaining Staff Wellbeing in Critical Care During and Beyond COVID-19 | Intensive Care Society | Outlines support mechanisms that should be considered to sustain wellbeing of staff in critical care during and beyond COVID-19. |
| Top Ten Messages for Supporting Healthcare Staff during the COVID-19 Pandemic | Williams R, Murray E, Neal A & Kemp V. 2020 | Guidance for leaders, clinical, and general managers on how to respond to the needs of staff and provide them support during COVID-19. |
| Guidance for planners of the psychosocial response to stress experienced by hospital staff associated with COVID: Early Interventions | Camden’s Traumatic Stress Clinic and Islington NHS Trust COVID Trauma Response Working Group | Guidance outlining early interventions and psychosocial response to stress experienced by hospital staff as they respond to COVID-19. |
Three Priority Needs
While workforce needs during the COVID-19 response have been vast and varied, hospitals and health systems have sought to address three priority needs. This table provides information about the priority aims and lists examples on the right.
- Meeting basic daily needs including food, housing options, transportation to/from work, personal safety including personal protective equipment, and childcare
- Enhancing communication for delivery of current, reliable, and reassuring messages
- Psychosocial and mental health support options
Considerations for Distinct Parts of the Workforce
While the COVID-19 response has impacted all members of the healthcare workforce, certain sub-populations may have experienced unique stressors that necessitate distinct considerations. This page defines these populations and provide resources that may be helpful.
To support member efforts in this area, GNYHA has curated this resources. Resources are organized into three sub-areas:
- Frameworks and Guides to Support Staff Well-Being/Emphasis on Post-Crisis and Return to Work
- Toolkits and Training Resources
- Psychoeducational Tools
If you have questions about any of these tools or would like assistance with you staff wellbeing support initiatives, please reach out to Jenna Mandel-Ricci or Catrina “Cat” Caneda.